Abstract
Background: Allogeneic HCT can be curative for certain subgroups of patients with AML. However, the financial burden of HCT is significant, and no studies have examined trends in cost over the last decade. We use the NIS, a nationally representative sample of hospital discharges in the US, to describe morbidity, mortality and cost of HCT in adults with AML.
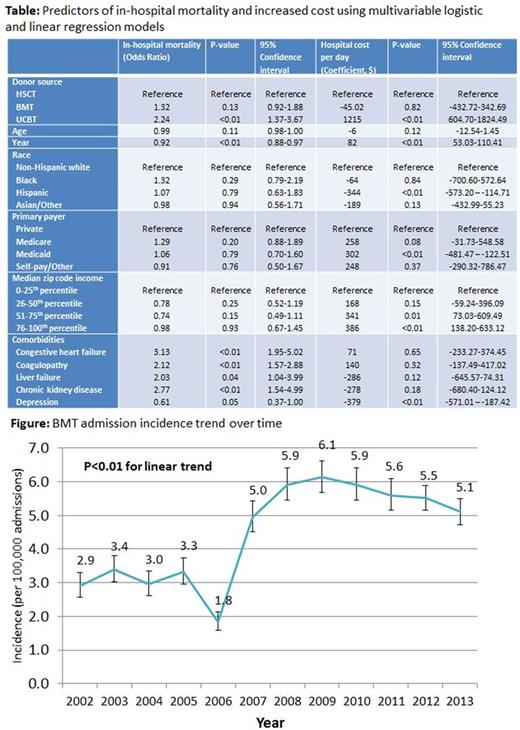
Methods: Years 2002-2013 of the NIS were queried for patients aged 18 and older with a primary procedure code of allogeneic hematopoietic stem cell transplant (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 41.00, 41.02, 41.03, 41.05, 41.06, 41.08) and a primary diagnosis of acute myeloid leukemia (ICD-9-CM codes 205.0, 205.2, 205.3). Mortality, length of stay, hospital costs, and complications were analyzed over the 12-year period. Subgroups based on type of transplant (Peripheral blood stem cell transplant (PBSCT), bone marrow transplant (BMT), and umbilical cord blood transplant (UCBT)). Predictors of mortality and cost were identified using multivariable regression models. Cost was derived from total hospital charges which were converted to cost using the provided NIS cost-to-charge ratios and adjusted for inflation using the 2013 Consumer Price Index.
Results: From 2002-2013, an estimated 19,965 adults with AML were admitted for HCT. Most (79%) had peripheral blood stem cell transplants (PBSCT); 15% had bone marrow transplants (BMT); 6% had umbilical cord blood transplants (UCBT). Twenty-seven percent of patients were aged 18-40, 49% aged 41-60, and 24% aged 61 and older. Most patients (81%) identified as non-Hispanic white; 5% identified as black, 7% as Hispanic; and 7% as Asian/other. Private insurance was the most common primary payer (68%), followed by Medicare (15%), Medicaid (11%), and Self-pay/Other (6%). The vast majority (97%) of hospitalizations took place at an urban teaching facility. Donor type (related versus unrelated) was not reported in 35% of PBSCT and 47% of HCT patients. Incidence of BMT (per 100,000 admissions) increased from 2.9 in 2002 to 5.1 in 2013 (Figure). Median length of stay was 26 days (Inter-quartile range (IQR), 22-33) for PBSCT, 28 days (IQR, 24-36) for BMT, and 35 days (IQR, 26-48) for UCBT. In hospital mortality was 8%, and did not differ significantly by age group (9% in patients 18-40, 7% in patients 41-60, and 8% in patients 61 and older). Mortality did significantly improve over the 12 year period (P<0.01 for linear trend). In-hospital mortality was significantly higher in the UCBT cohort (15%) compared to PBSCT (7%) (P<0.01) and BMT (10%) (P=0.03). Major complications included: stomatitis (36%), total parenteral nutrition (17%), neutropenic fever (14%), bacteremia (12%), mechanical ventilation (6%), and dialysis (3%). Upon univariate regression analysis, compared to PBSCT, UCBT patients were less likely to experience stomatitis (OR=0.60, P<0.01), but more likely to experience sepsis (OR=2.06, P<0.01), bacteremia (OR=2.08, P<0.01), disseminated Candida infection (OR=4.47,P<0.01), and mechanical ventilation (OR=2.15,P<0.01). Median hospital costs for the entire cohort were $96,478 (IQR, $66,460-$143,495). Average daily cost increased significantly over time (Coefficient=$68, P<0.01 for linear trend). UCBT incurred a median cost of $161,855 (IQR, $113,613-221,944), while PBSCT and BMT incurred median costs of $92,923 (IQR, $64,074-137,421) and $98,601 (IQR, $67,697-$142,220), respectively. After adjustment for socio-demographic factors and comorbidities, UCBT was associated with increased mortality (OR 2.25, P<0.01) and cost (coefficient $1,215, P<0.01) relative to PBSCT (Table). BMT did not significantly increase mortality or cost compared to PBSCT.
Conclusions: This study demonstrates that initial costs for inpatient allogeneic HCT have increased significantly since 2002, while mortality has improved. It also demonstrates increased cost and mortality with umbilical cord transplants compared to PBSCT even after adjustments for socio-demographic factors and comorbidities. This is likely secondary to an increased risk of severe in-hospital complications in patients undergoing UCBT. Further research is needed to explain the increased morbidity, mortality and cost associated with this particular group.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal